
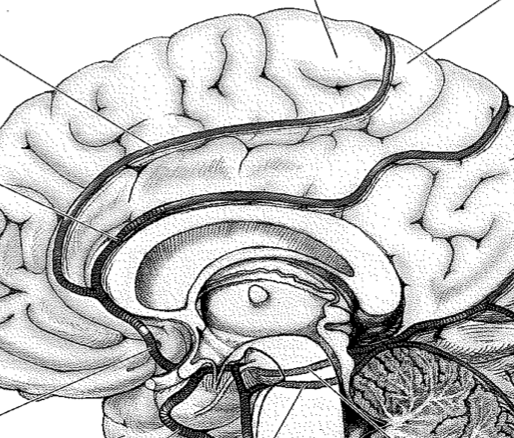
Vascular Anatomy
- Anatomy Review
- CT Angiogram (axial)
- CT Angiogram (coronal COW)
MCA Syndromes

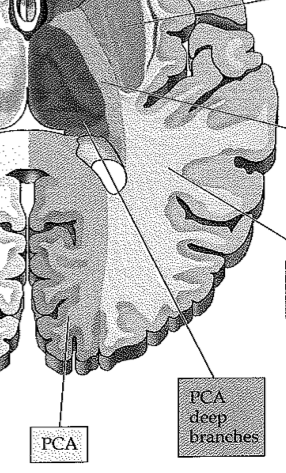
PCA Syndromes
ACA Syndromes
Lacunar Syndromes
Brainstem Syndromes
- Brainstem lesions classically produce "crossed deficits"
- unilateral cranial nerve deficits with contralateral motor/sensory deficits ("long tract signs")
- ...the reason to learn brainstem syndromes is to understand neuroanatomy, not because they are commonly encountered in clinical practice!
Thalamic Syndromes
- Vascular syndromes of the thalamus (table)
Cases
Case One
- 80 yo F with PMHx of A. Fib, HTN, T2DM, dyslipidemia, obesity
- acute onset of confusion, decreased movement of left arm and leg
Case Two
- 87 yo F with PMHx of A. Fib, HTN, dyslipidemia, obesity
- Presented to ER 2 hours from symptom onset with speech difficulty, right-sided weakness
- treated with IV tPA in the emergency department
- symptoms improving the next day, with improvement of language but ongoing right-sided weakness
Case Three
- 72 yo M farmer with PMHx of HTN, smoking, dyslipidemia
- Presented with a three day history of right-sided weakness
Case Four
- 73 yo M with PMHx of HTN, PVD, impaired fasting glucose, mild cognitive impairment
- Presents with diplopia, dysarthria, and right-sided weakness
Case Five
- 74 yo M with PMHx of HTN, smoking, A. Fib, surgical repair of spinal dural fistual (residual Rt LE weakness with upgoing toe)
- Presents with 4 day history of nausea, vomiting, malaise
- 3 days ago - gait ataxia
- On the day of presentation, ataxia worsening, fell at home, came to hospital
- Denied headache, neck pain, or recent trauma
Case Six
- 77 yo M adm to hospital with mild right-sided weakness and global aphasia, treated with IV tPA
- 2 days after admission, he had a seizure and required intubation for decreased LOC
- off sedation, he was confused, with severe right-sided hemiparesis
Case Seven
- 79 yo M found down by his son in the garage
- Last seen well the night before
- Had managed to shovel the sidewalk before he collapsed

References
references in bold are highly recommended
- Marx, J. J., & Thömke, F. (2009). Classical crossed brain stem syndromes: myth or reality? Journal of Neurology, 256(6), 898–903. doi:10.1007/s00415-009-5037-2
- Schmahmann, J. D. (2003). Vascular syndromes of the thalamus. Stroke; a journal of cerebral circulation, 34(9), 2264–2278. doi:10.1161/01.STR.0000087786.38997.9E
- Blumenfeld, H. (2002). Neuroanatomy through Clinical Cases, 1–480.
- Haines, D. E. (2008). Neuroanatomy. Lippincott Williams & Wilkins.