1. What are the levels of the systems approach, their associated research fields, and the nature of problems and unique matters at each level?
2. What went wrong with the Therac-25 device, and why?
3. What are iatrogenic injuries, what is their incidence, and why do they occur?
4. What are the different types of medical errors? What are the unique challenges associated with error in medicine?
5. Can human error ever be good?
6. Describe some future directions for HF/E.
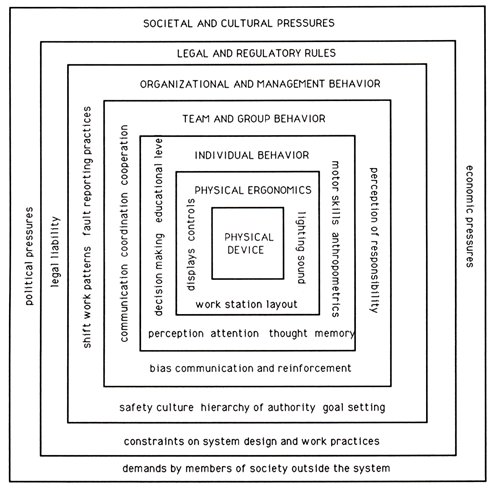
(e.g., Moray, 1994)
Definition: A means of understanding the structure and function of a complex system by describing and explaining the interaction of its components, and the system’s role within an environment, at all different levels of analysis. It is a sociotechnical approach that characterizes the interaction between people and technology in workplaces.
Related to systems thinking and systems science.
Level 1. Physical _______ & Physical __________: the design & the immediate environment
- research fields: industrial design, engineering; anthropometry
- includes design model/designer’s conceptual model and system image
- nature of error: poor design ignoring human physical capacities can induce errors, cause RSIs, etc.
- unique issues:
• universal design of displays, controls, etc.
• effects of ambient/environmental factors: illumination, humidity, temperature, noise, etc.
Level 2. __________ Behaviour: the actor
- research field: psychology (perception, cognition, emotion, motor control)
- nature of error: blame frequently attributed to “human error,” masking the effects of contributing causes at other levels
- unique issues:
• fallible memory, reasoning, decision making, stress
• effects of illusions, slips, mistakes, etc.
Level 3. Team & _____ Behaviour: the interpersonal context
- research fields: social psychology, sociology
- includes communication
- nature of error: poor communication; flawed group decision-making; groupthink
- unique issues:
• development of psychological safety
• __________ cannot be applied to people; diffusion of responsibility decreases reliability of group
Level 4. Organizational & __________ Behaviour: structure and supervision
- research fields: industrial and organizational (I/O) psychology, management theory
- includes cultivation of safety culture
- nature of error: mismanagement; faulty policies
- unique issues:
• in a hierarchy, those at upper levels may lack technical expertise to confirm work done properly by those at lower levels
• management creates policy, which affects entire organization
e.g., decision to go to 24-hour shiftwork, investment in design, should errors be punished or investigated?
e.g., about 20% of profitability is determined by error management culture (van Dyck et al., 2005)
Level 5. _____ & Regulatory Rules: laws and rules
- research fields: forensic psychology, legal scholars, governments?
- includes laws that restrict behaviour, and incentives (like tax cuts) that encourage behaviour
- nature of error: lack of appropriate oversight; legal liability; violations contravene laws or rules
- unique issues:
• too many rules; difficult to know them all
• less than half of people read a contract or legal document before signing it
• legislation lags behind technological developments
• loopholes: letter of the law may be observed, but not the spirit in which it was intended
• in a lawsuit or trial, blame is often assigned--falling at the feet of an __________
Level 6. ________ & Cultural Pressures: the larger social context
- research fields: cultural psychology, cultural anthropology, sociology; economics, political science
- includes economic and political pressures
- nature of error: misunderstanding due to cultural differences, political ideology; insufficient monetary resources
- unique issues:
• different viewpoints provided by cultural beliefs, practices, customs, social norms, and institutions
____________ among all levels must also be considered.
Implications: people will make errors, so change other parts of the system:
• redesign human-machine __________; improve environmental conditions
• reduce ________; enhance wellness
• improve _____________
• decrease ________ to stay on time/on budget; foster safety culture
• consider safety legislation; promote awareness
• understand cultural, economic, and political factors
Casey (1998):
Background
- medical linear accelerator made by Atomic Energy of Canada Limited (AECL)
- delivers radiation beam to patient to remove remnants of _________ growths or tumours after surgery
- treatment usually involves many low-energy dosages over successive treatment sessions
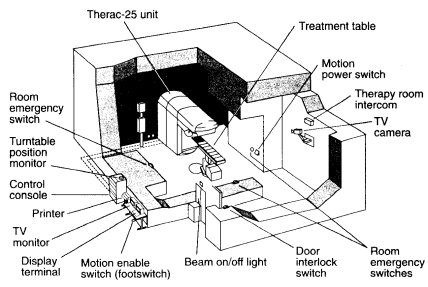
- dual modes:
1. ___-______ mode: electron beam of 5-25 MeV (million electron volts) aimed directly at patient and sent off in a short burst; used to treat shallow tissue
2. high-energy _-___ mode: uses full 25 MeV capacity of the machine; used to reach deeper tissue
• for “electron mode”, technician types “e”; for “X-ray mode”, technician types “x”
• for X-ray mode, arm moves tungsten plate between beam source and patient
• beam passes through plate ![]() transformed into X-ray
transformed into X-ray
- machine controlled via DEC VT100 terminal connected to PDP-11 mainframe computer located in another room
- ________ was responsible for maintaining safety, including monitoring electron-beam scanning (previous models had hardware interlocks)
- Therac-25 software modified from Therac-20
The case of Texas oil worker Ray Cox: March, 1986
- went in for 9th electron beam treatment on his shoulder
- technician entered ____________ into terminal: 22 MeV electron-beam treatment of 180 rads
- moved cursor to next entry field, hit “x” to set the mode
- realizing she made a mistake, she hit “![]() ” key, selected “Edit” command, “e” for Electron beam, then “Enter” (took < 8 s)
” key, selected “Edit” command, “e” for Electron beam, then “Enter” (took < 8 s)
- system showed “Beam Ready” prompt; tech hit “b” key
- message was displayed: ___________ __
- sheet on machine listed this “____ _____ 2” error (dose too high or low)
- tech cleared error display, hit “b” again: same error
- third time: same error message
- Ray felt repeated burning, stabbing _____; the third time, he pulled himself off the table
Results
- Ray ____ of complications from the overdose 5 months later
- problem not diagnosed until 3 weeks later; same thing happened to another patient
- senior tech reported situation to manufacturer; six similar overdoses in Georgia, Washington, and Canada
- machine ________ in 1987
Causes
1. physical device:
• Therac-25 could not properly monitor setup and radiation exposure to prevent disaster
• error messages gave poor feedback
2. individual behaviour:
• ________ error: decision-making
- technician misinterpreted situation ![]() chose inappropriate procedure
chose inappropriate procedure
• __________ error: software bug (latent error)
- if command sequence executed too quickly, a “race condition” occurred: two sets of instructions were sent, and the first one to arrive set the mode
- arm correctly withdrew tungsten plate, but energy level was not reduced
- machine (apparently) in electron mode, but was actually in a hybrid high-energy mode
- system delivered 25,000 rads with 25 MeV (>125× normal)
- this keystroke sequence had never been tested
3. team & group behaviour: poor communication
• intercom between patient and tech was broken, and video hookup between rooms was disconnected
• company failed to tell its users/customers about this problem
4. organizational & management behaviour: safety culture
• inadequate reporting structure in company
• poor safety engineering:
- error condition detected, but insufficiently informative
- operator’s manual did not explain malfunction codes
5. legal & regulatory rules:
• Therac-25 skipped FDA testing due to its similarity to Therac-20; incidents prompted only a _________ Class II recall by FDA
• lawsuits filed by victims’ families were settled out of court
6. societal & cultural pressures
• computer-controlled dual-mode device reduced ____--but introduced greater complexity
• expectation of error-free health care
To err is human: Building a safer health system (Kohn, Corrigan, & Donaldson, 2000):
- report released by Institute of Medicine, National Academy of Sciences
- focused on __________ injury: caused by a physician or other health-care provider
- analyzed previous data on medical error
• Harvard Medical Practice Study (Brennan et al., 1991; Leape et al., 1991):
▸ chart review of NY state hospital data from 1984
▸ found 3.7% of patients experienced an _______ _____ (AE) caused by treatment
▸ of these, 58% were caused by ______; 14% were fatal
▸ __________ errors occurred in 2-14% of patients, but most did not result in injury
• Utah/Colorado study (Thomas et al., 1999):
▸ found 2.9% rate of AEs
- estimated 44,000-98,000 deaths/year due to iatrogenic injuries in hospitals (8th leading cause of death in US in 1999)
- most iatrogenic injuries are due to _____; errors are preventable
- cost = US$29 billion per year
- criticisms:
![]() eliminating AEs may not prevent deaths
eliminating AEs may not prevent deaths
![]() NY data focused on patients with a high likelihood of AEs
NY data focused on patients with a high likelihood of AEs
- results of IOM report:
• President Clinton directed Quality Interagency Coordination Task Force (QuIC) to develop a strategy
• Patient Safety and Quality Improvement Act enacted in 2005; created blame-free adverse event reporting
- updates:
• To Err is Human — To Delay is Deadly: Ten years later, a million lives lost, billions of dollars wasted (Jewell & McGiffert, 2009):
▸ argued for greater change to improve the health-care system
▸ e.g., use of a _________ for inserting a central line reduced infections by 66%--saving 1,500+ lives, and $200 M over 18 months
• update based on 2008-2011 data (James, 2013):
▸ “preventable harm” estimated to result in 210,000 to 400,000 deaths/year
• however, a more recent systematic review and meta-analysis of studies started with hospital deaths and worked backward to ascertain their causes (Rodwin et al., 2020):
▸ rate of preventable mortality was 3.1%
▸ this corresponds to about 12,165 deaths/year in the US
Unique issues in health care:
• _______________
- high tech instruments are complex; have many controls
• ____/test reports
- may be ignored, misplaced, forgotten
- results may vary
e.g., “_____-____ hypertension” (elevated blood pressure found only in clinical situations, due to patient anxiety) affects about 5% of patients
• ________-______ process
- based on patient self-reports (but what is relevant?)
- affected by biases
• __________ & prescriptions
- contraindications, side effects, interactions (with other drugs, or foods)
e.g., grapefruit-drug interactions (Bailey et al., 1989); licorice-drug interactions (Foster et al., 2017)
- sound-alike or easily confused written drug names
e.g., name of proton pump inhibitor Losec® changed to Prilosec® in the US after fatal confusions with diuretic Lasix®
Solutions: hand-print orders/prescriptions, computerized physician order entry (CPOE), use bolded “____ ___” capital letters
(e.g., acetoHEXAMIDE is less likely to be confused with acetaZOLAMIDE)
- _____________ on prescriptions can be confusing or ambiguous; 4.7% of medication errors involve abbreviations (Brunetti et al., 2007)
e.g., “qd” (every day) may be misread as “qid” (four times a day)
Solution: the words “every day” should be spelled out
• _________
- errors often not reported, thus are seen as isolated; “flukes”
- AEs often have no lasting harmful effects
- malpractice insurance is expensive, thus errors are not avowed (doctors told to “deny and defend”)
▸ 85,000 medical malpractice lawsuits filed per year (US data)
▸ lawsuits cost $11-$29B per year
▸ account for 5-9% of hospital expenditures
- result: potential _______ _______ (“defensive medicine”: the practice of diagnostic or therapeutic measures conducted primarily not to ensure the health of the patient, but as a safeguard against possible malpractice liability)
- if errors are _______ to occur, means can be sought to study, prevent, and reduce them, and minimize their consequences
- if errors are not assumed to occur...?
Leape (1994): types of medical errors
1. _________: 21.9%
• failure to employ indicated tests
• misreading lab results
• failure to act on results of monitoring or testing
e.g., stomach pains = ___________?
2. _________: 60.5%
• performance error
• error in preparation/dosage
• delayed treatment or inappropriate care
e.g., nicking an ______ during surgery
3. __________: 16.2%
• failure to provide ____________ treatment
• inadequate monitoring
• inadequate follow-up of treatment
e.g., not prescribing antibiotics after oral surgery
4. _____: 1.2%
• equipment failure
• poor communication in situated environments
(e.g., ER, OR, ICU)
e.g., amount of drug given is not recorded
- more than 75% of errors were preventable
- most errors due to mismanagement of patients--not due to rare conditions or negligence (failing to meet the ordinary standard of care)
Lesar et al. (1990):
- analysed medication errors in NY teaching hospital
- overall rate: 3 per 1,000 prescriptions; 1.8 were “significant”
- most common types:
• ________: 41.8%
• underdose: 16.5%
• allergy: 12.9%
• wrong dosage ____ (e.g., if patient is vomiting, they should not receive medication in oral dosage form, but inhalational or suppository instead): 11.6%
• wrong drug: 5%
• duplicate therapy (e.g., prescriptions for two medications from the same class): 5%
• wrong _____ (e.g., flu shot must be given intramuscularly, not intravenously): 3.3%
• wrong _______: 0.4%
Patient safety in Canada:
• Baker, Norton, et al. (2004): Canadian AE Study
- reviewed charts from hospitals in BC, AB, ON, QC, NS
- AE rate was ___%
- 36.9% were judged preventable
- mortality rate was 20.8%
• Canadian Patient Safety Institute (CPSI) established 2003
• Health Quality Council of Alberta (HQCA) established 2002
• only 8 of 13 provinces & territories have adverse event reporting laws; Alberta does not (Milligan et al., 2021)
• 5.9% of hospitalizations in 2021-2022 (about 140,000 out of 2.4 million hospital stays) resulted in a harmful event requiring treatment or a longer hospital stay (CIHI, 2023)
__________ & Hamilton (2001): Medical Error Description study
- questionnaires given to 97 medical residency candidates
- 25 questions on ___________ of errors
- most common error type:
slip |
60.3% |
mistake |
20.6% |
both |
7.4% |
- severity of most errors:
none apparent |
23.5% |
slight/no treatment |
45.6% |
slight/minor treatment |
26.5% |
moderate |
1.5% |
serious |
0.0% |
- most problematic shift:
6 a.m.-noon |
11.5% |
noon-6 p.m. |
19.7% |
6 p.m.-midnight |
26.2% |
midnight-6 a.m. |
41.0% |
- percentage of problems due to medication: 49%
- most problematic meds:
• ___________: 32.6%
• cardiac/cardiovascular: 16.3%
• analgesics: 14.3%
- percentage of errors due to miscommunication: 45.7%
- why not reported?
• minor/no consequences/problem fixed: 61.4%
• fear of consequences: 22.8%
Leape (2004): barriers to change
• __________
- of technologies, operations, and relationships
• culture of _____ and _____
- physicians held to a standard of perfection
- thus, errors seen as result of __________
- are treated as “dirty secrets” at closed-door morbidity and mortality (M&M) conferences
- solution: disclosure and _______
▸ University of Michigan Health System: existing claims and lawsuits dropped from 262 to 83
▸ University of Illinois Medical Center: malpractice filings dropped by half (out of 37 apologies for preventable errors, only 1 patient filed suit)
▸ in Colorado, malpractice claims dropped 50% since 2000
▸ Beth Israel Deaconess Medical Center in Boston: 35% decrease in ___
▸ as of 2009, 36 states had “apology laws”; malpractice payments in these states were 14-17% lower ($55,000-$73,000)
• misguided _______________
- overemphasis on technical skills, at the expense of training in teamwork or “soft” sciences
• lack of organizational _______
- hospital/state/national oversight is piecemeal
- little standardization (“critical condition” vs. “serious condition”?)
- inadequate development/use of IT
• lack of organizational commitment to ______
- no formalized, systematic review process
- individualized review process: cause in ______ not determined
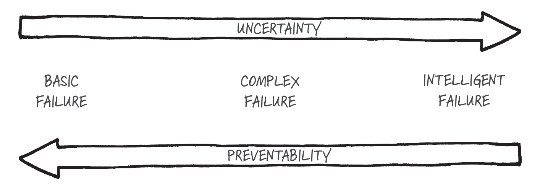
Can human error ever be good? (Edmondson, 2023)
• _____ failure: occurs in consistent environment and has a single cause; due to inattention, neglect, overconfidence, faulty assumptions
e.g., on a vehicle assembly line, a worker accidentally installs a part incorrectly
• _______ failure: happens in familiar settings, but factors combine in novel ways; has multiple causes; often involves external factors; preceded by warning signs
e.g., a surgical complication occurs due to a series of unforeseen circumstances align in a catastrophic way: the patient has an unexpected reaction to anesthesia, and they have with a rare blood type that leads to complications in surgery
• ___________ failure: takes place in novel situations, driven by opportunity; informed by prior knowledge; consequences are minimized
e.g., in a scientific laboratory, an experiment to test a new drug turns out not to work
• Problems cognitive engineering has inherited from cognitive psychology (Landauer, 2003):
- abstract theories studied, instead of ________ applications
- subtle psychological effects have been most studied; more data on ______ effects needed
- principles of cognition rarely influence machine ______
- designers are largely _______ of cognitive principles
• _______________: study of the brain and behaviour in work contexts (Parasuraman & Rizzo, 2007)
- considers brain function and the neural bases of cognitive processes and performance in real-world tasks
- applies existing and emerging knowledge of human performance and brain function to design systems for safer and more efficient operation
- research has increased with greater availability of brain imaging technology
• Environmentally ___________ design and climate ergonomics (Norman, 2023; Chartered Institute of Ergonomics & Human Factors, 2021)
- climate change has been profoundly affected by designed objects
e.g., disposable products, electronics that cannot be repaired, pollution-causing vehicles
- the field of design should also play a role in reversing this problem
- goal is to optimize both human, environmental, and climate well-being
• Technology ____: innovations in applying technology to the workplace are driving changes to the nature of human work
- influences the direction and growth of HF/E
- artificial intelligence and automation have implications for the world of work
e.g., ChatGPT, autonomous vehicles, robotic surgical systems
- people will have to learn new skills (human-_____ interaction, human-AI teaming)
- will the technology be appropriately adapted to ______?
Kim Vicente. (2004). The human factor: Revolutionizing the way people live with technology. Alfred A. Knopf Canada.
Marc Gerstein. (2008). Flirting with disaster: Why accidents are rarely accidental. Union Square Press.
Fran Locher Freiman & Neil Schlager. (1997). Failed technology: True stories of technological disasters (2nd ed.). Gale Research Inc.
Victor Lombardi. (2013). Why we fail: Learning from experience design failures. Rosenfeld Media.
Stephen Casey. (1998). Set phasers on stun and other true tales of design, technology, and human error (2nd ed.). Aegean.
Stephen Casey. (2006). The atomic chef: And other true tales of design, technology, and human error. Aegean.
Jonathan Shariat & Cynthia Savard Saucier. (2017). Tragic design: The true impact of bad design and how to fix it. O’Reilly Media.
Atul Gawande. (2009). The checklist manifesto: How to get things right. Metropolitan Books.
Asaf Degani. (2003). Taming HAL: Designing interfaces beyond 2001. Palgrave Macmillan.
Alan Cooper. (2004). The inmates are running the asylum: Why high-tech products drive us crazy and how to restore the sanity (2nd ed.). Sams.
Jakob Nielsen & Hoa Loranger. (2006). Prioritizing web usability. New Riders.
Jeff Johnson. (2020). Designing with the mind in mind: Simple guide to understanding user interface design guidelines (3rd ed.). Morgan Kaufman.
Edward R. Tufte. (1990). Envisioning information. Graphics Press.
Edward R. Tufte. (1997). Visual explanations: Images and quantities, evidence and narrative. Graphics Press.
Edward R. Tufte. (2001). The visual display of quantitative information (2nd ed.). Graphics Press.
Donald A. Norman. (1999). The invisible computer: Why good products can fail, the personal computer is so complex, and information appliances are the solution. The MIT Press.
Donald A. Norman. (2004). Emotional design: Why we love (or hate) everyday things. Basic Books.
Donald A. Norman. (2007). The design of future things. Basic Books.