1. What are habits, and what differentiates them from other behaviours?
2. How are habits different from habit disorders?
3. What are some habits?
4. Describe the components of habit reversal training.
5. What are some other habit-change procedures?
6. How is habit reversal applied?
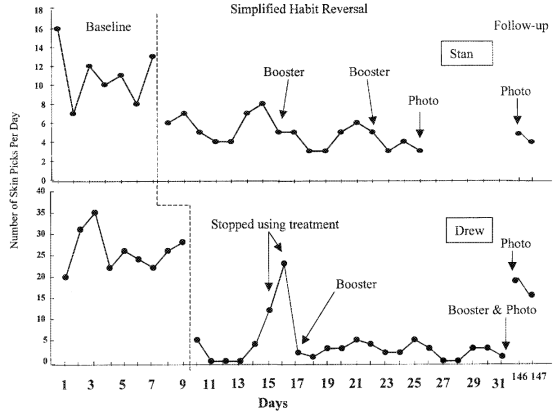
How can habit reversal be used to reduce skin picking?
(Twohig & Woods, 2001)
- two adult male siblings, Stan (20 years old) and Drew (22 years old)
- target behaviour was skin picking: digging their fingernails into their fingertips, and pulling or scraping the skin causing bleeding and scarring
- behavioural treatment program:
1. each client worked with the therapist to:
• describe skin picking of fingers and its ___________, such as rubbing the fingers
• recognize the therapist’s simulation of the antecedent and problem behaviours
• ___________ his own antecedent and picking behaviours, and their consequences
2. perform fist clenching for 1 minute when an antecedent or target behaviour occurred
• therapist modeled this first
• clients practiced it after each simulation
3. given periodic _______ sessions to refresh this training
- clients self-monitored their target behaviour
- photos of their fingers were also taken periodically
- results:
• target behaviour declined
• photos revealed their hands showed ____ damage
“All our life, so far as it has definite form, is but a mass of habits” (William James, 1892, p.64)
It has been estimated that more than __% of the actions people perform each day are habits (Neal et al., 2006; Verplanken & Wood, 2006).
Prevalence of habits in a survey of college students (Woods et al., 1996):
• ____ manipulation: 15%
• hair pulling (trichotillomania): 3%
• nail biting (onychophagia): 10%
• chewing on their mouth, lips, or cheeks: 22%
• ____________ objects such as pens, pencils, or jewelry: 22%
• teeth grinding (bruxism): 5%
- definition: (bad) habits are repetitive or stereotyped behaviours (persistent postural, gestural, or verbal responses) that serve no useful purpose and tend to be an annoyance
e.g., motor tics, stuttering, and nervous habits (like nail biting, lip biting, etc.)
- occur automatically/subconsciously
- are cued by aspects of the performance context (i.e., environment, preceding actions)
- are learned through a process of repetition, so that they are stored in __________ memory (memory subsystem that supports minimally conscious control of skilled action)
- involve the ________ of the basal ganglia, which is also associated with voluntary motor control and procedural learning (Seger & Spiering, 2006)
- are often maintained by _________ reinforcement
Rapp et al. (1999):
- Kris, a 19-year-old woman with cerebral palsy and moderate intellectual impairment
- target behaviours: hair pulling and hair manipulation
- in the literature, hair pulling is often attributed to _________ states, which are unobservable
- functional analysis:
• ______: Kris made to do paper-sorting task
• attention: therapist gave social reinforcement contingent on target behaviours
• _____: Kris watched TV while being videotaped
• control: Kris played with toys in a room with the therapist
- results: target behaviours occurred only in alone condition
• target behaviours disappeared when Kris wore latex ______
• thus, digital-tactile stimulation served as automatic positive reinforcement
- the DSM-5-TR (2022) does not have a habit ________ category
- a behaviour may be loosely characterized as a disorder if it:
• is distressing to the person
• occurs with sufficient frequency or intensity to cause the person to seek _________
• has adverse physical (i.e., tissue damage) or social (i.e., embarrassment, social stigma) effects on the person
• _______ habits: repetitive, manipulative behaviours that are assumed to occur when a person experiences heightened nervous tension
e.g., fingernail biting, teeth grinding, thumb sucking
- also called body-focused repetitive behaviours (BFRB)
- originally believed to reduce nervous tension or _______; are known to be induced by boredom, frustration, or stress, or serve as self-stimulation
- are associated with perfectionism (which causes frustration and stress) (Roberts et al., 2015)
• _____ tics: repetitive, jerking movements of the body
e.g., facial tics, head jerking
- may be due to increased muscle tension
- a certain movement may produce relief to injured area, but tic persists even after injury has healed
• _____ tic: repetitive nonspeech vocal sound that does not convey information or serve a social function
e.g., excessive throat-clearing, or uttered sounds
• Tourette’s disorder/syndrome: includes ________ motor tics and at least one vocal tic
- only a small minority of those with Tourette’s utter obscenities, socially inappropriate or derogatory remarks
- caused by interaction of genetic and environmental factors
- often presents with other ________ factors, such as ADHD (attention-deficit hyperactivity disorder) or OCD (obsessive-compulsive disorder)
- typically not treated with medication, but with behavioural therapies (e.g., using DRO)
• __________: speech dysfluency in which a person repeats syllables or words, prolongs the length of a syllable or word, or experiences blocking (inability to produce the sound)
- many behavioural therapeutic treatments exist, including breathing exercises, fluency shaping, and stuttering modification therapy
- definition: methods for decreasing habit behaviours that do not employ _____________; typically are applied by the client while under the guidance of a behaviour analyst
- first developed by Nathan H. Azrin and R. Gregory Nunn (1973)
- comprised of two main components:
• _________ training: person is taught to describe the problem behaviour, and then to watch for it and notice when it occurs (or is about to occur)
• _________ response training: person is taught to perform a behaviour that is incompatible with the target behaviour
e.g., for nail-biting behaviour, the person is instructed to put their arms at their sides and make their hands into fists when they feel like biting their nails
- competing response both prevents the target behaviour and provides an alternative behaviour
- competing response may serve as ________ when it is performed after the target behaviour
- usually, the response is unobtrusive
- the optimal duration of a competing response is 1-3 minutes (Twohig & Woods, 2001)
- HRT may also apply:
• ______ support: family members or friends who spend significant time with the target person:
▸ point out when the target behaviour occurs
▸ prompt the use of a competing behaviour
▸ and reinforce the competing response or a desirable behaviour
• __________ strategy: behaviour analyst works with client to determine situations and antecedents for the target behaviour, as well as consequences
▸ includes review of the drawbacks of the behaviour (e.g., embarrassment, skin damage)
▸ may include self-administered consequences (e.g., reinforcement with candy following a period without nail-biting)
▸ used to increase compliance with competing response
- applying HRT:
1. client learns to describe and ________ the problem behaviour
2. client learns and practices a behaviour that is incompatible with or ________ with the problem behaviour
3. for motivation, client reviews the adverse effects of the habit, records and graphs the behaviour, and has someone (e.g., a family member) provide reinforcement for engaging in the treatment
Note: More serious problems/psychological disorders require the application of cognitive behavioural (or other) _______.
Other procedures:
______________ training: practice focuses on how to control tics in everyday situations
- first, person practices tic-control procedures in session until done correctly
- ______ rehearsal: person imagines common and tic-eliciting situations and then performs the tic-control exercise
- finally, the person tries controlling tics in real-world situations
________ therapy: a form of respondent conditioning which involved the repeated pairing of a troublesome reinforcer with an aversive event
e.g., treatment of alcoholism:
• disulfiram (US) given with alcoholic drinks (NS) interacts to cause nausea and other extremely __________ reactions (UR)
• repeated pairings of alcohol with disulfiram may cause the person to avoid alcohol (CS)
- has been applied to alcoholism, cigarette smoking, nail-biting, substance abuse, homosexuality, “sexual ________,” and pathological gambling
- uses aversive stimuli like electric shocks, elastic/rubber bands snapped on the wrist, and covert sensitization (________ aversion)
- therapy often uses symbolic representations (e.g., pictures or videos) to replace the troublesome reinforcer itself
- often has a high dropout rate (e.g., only 1%-7% continue taking disulfiram)
- may work better in conjunction with a behavioural counseling program/behaviour therapy
- implementation requires special expertise
______ ________ practice: a punishment procedure that requires the person to repeat the undesired target behaviour for a predetermined time period contingent on the occurrence of the target behaviour
e.g., after a vocal tic, the person would have to force him or herself to make vocal tics for 2 minutes
- not the same as a competing response, which should prevent the target behaviour
- evidence indicates that massed negative practice is not as effective as HRT (Woods et al., 2006)
Weight Watchers
- commercial weight-loss program (not a ________ program)
- applies “Activity, healthy habits, support and smart food choices” to reduce weight
- users apply “SmartPoints®” to food selections in order to decrease calorie consumption
- may also attend in-person meetings
- obese people in Weight Watchers lost more weight vs. those assigned to a ____-____ group (Heshka et al., 2003)
• 4.6% vs. 1.7% after 1 year
• 3.1% vs. 0.2% after 2 years
Foster et al. (2005):
- behavioural treatment of obesity includes the use of:
• goal-setting
• ____ support
• physical activity
• nutrition education
• self-monitoring: keeping food and activity records
• _______ _______: identifying antecedents for overeating
• stimulus control: controlling cues associated with eating
• cognitive restructuring: cognitive _______
- evidence shows that self-monitoring is associated with better weight control in the short term
- but ________ activity is associated with better weight control in the long term
- behavioral treatment has been found to produce weight loss of 8-10% during the first 6 months of treatment