J Pharm Pharmaceut Sci (www.cspscanada.org) 8(2):332-334, 2005
Thrombolytic treatment as
first option in recurrent tricuspid prosthetic valve thrombosis and Ebstein’s
anomaly
Fidel Manuel
Cáceres-Lóriga1, Horacio
Pérez-López1, José
Santos-Gracia1, Karel
Morlans-Hernández1, María
A. Marrero-Mirayaga2.
1
Institute of Cardiology and Cardiovascular Surgery.
Received April 6 2005, Revised June 14 2005, Accepted June 28 2005, Published August 12 2005
Correspondence to: Fidel
Manuel Cáceres-Lóriga,
Instituto de Cardiología y Cirugía Cardiovascular. Calle 17 # 702 Esq. A. Vedado,
Plaza. CP 10400. Ciudad de
ABSTRACT
Ebstein’s
anomaly is the most frequent cause of congenital tricuspid regurgitation. The coexistence of a mechanical heart
prosthesis in a low-pressure circuit and poor compliance in the anticoagulant
therapy contributed decisively to the appearance of recurrent mechanical heart
valve thrombosis in these patients. A 49 years old female patient is reported
where thrombolytic therapy with recombinant Streptokinase (TT-rSK) was the
first treatment choice in seven recurrent episodes of prosthetic valve
thrombosis.
INTRODUCTION
An
abnormal junction of the bicuspid valves
produces
a pathological descent of the tricuspid valve in the right ventricle
characterizing Ebstein’s Anomaly (EA). According to the degree of tricuspid regurgitation
or the association of other malformations, the clinical picture of this disease
ranges from the absence of symptoms to severe heart failure. In case surgical
treatment is required, its success would depend upon the possibility of
reconstruction (or replacement) of the tricuspid valve (TV) (1, 2).
A patient is reported with EA who has undergone three tricuspid valve
replacements, and has suffered eight episodes of prosthetic heart valve
thrombosis that has been treated with thrombolytic drugs in the course of 7
years.
The main purpose of this paper is report a case where multiple courses
of thrombolytic treatment were used for prosthetic heart valve thrombosis as
first therapeutic option.
CLINIC CASE
We
present a 49 year old female patient, diagnosed at age 31 with an EA, atrial
septal defect (ASD) and severe tricuspid regurgitation. She was operated on to
close the ASD and right atrial plicature and to replace the TV by a
bioprosthesis. Four years later, the bioprosthesis degenerated and was replaced
by a monodisc mechanical prosthesis. Warfarin was maintained as anticoagulant
therapy. Four years later, the patient was admitted with right cardiac failure
and reported absence of prosthetic sounds. The transthoracic echocardio-gram
(TTE) revealed a thrombosis of the tricuspid prosthesis (increase of
echogenicity in the auricular side of the prosthesis and a marked decrease of
the movements of the disc).
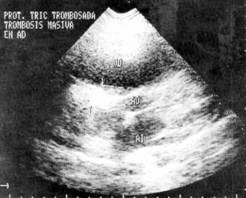
Figure
1: Trans-thoracic echocardiogram
where a tricuspid prosthesis is observed with increase in its echogenicity that
extends toward right atrium corresponding to a massive thrombosis.
With the consent of the patient, a thrombolytic treatment (TT) with
recombinant streptokinase (rSK), baseline doses of 250,000 IU in 30 minutes
followed by a continuous infusion of 100,000 IU/hour, was initiated lasting 48
hours. The total doses administered were 5,000,000 IU.
The symptoms disappeared and the TTE showed a total disappearance of the
thrombus and a recovery of the disc movements. There were no complications due
to the thrombolytic therapy.
After this episode, the
patient further experienced seven similar crises of rethrombosis. They all
responded to therapy. In the last episode, despite the disappearance of the
symptoms, hepatomegaly and ascitis remained. A non-obstructive residual image
was observed in the heart prosthesis after thrombolysis, so the valve had to be
replaced again. Abundant pannus was observed around the prosthesis. Presently,
two years after the surgical procedure, the patient remains asymptomatic.
DISCUSSION
Ebtein’s anomaly is the most frequent cause of congenital tricuspid
failure. The magnitude of the tricuspid failure, together with the extension of
the atrialized right ventricle, determines the degree of deterioration of the
right ventricular function. The coexistence of a mechanical heart valve
prosthesis in a low pressure circuit and irregularities in the anticoagulant
therapy contributed decisively to the appearance of recurrent prosthetic
thrombosis in this patient (3).
We reported a previous series of
cases where tricuspid heart valve thrombosis was involved (4) and TT prescribed with good results.
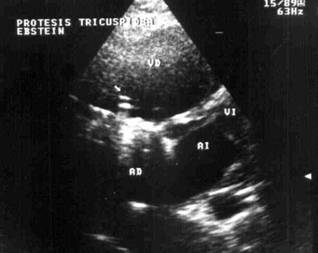
Figure 2: Trans-thoracic echocardiogram,
in the same tricuspid prosthesis where you can see that thrombus has
disappeared and normal functioning of the mechanical prosthesis 72 hours after
thrombolysis.
There was agreement with
others (5-7), in considering
thrombolysis as the treatment of choice. In these patients with high thrombotic
risk, the antithrombotic prophylaxis and the adequate follow-up of the
anticoagulation are extremely important. In case any thrombotic complication
occurred, there should be no doubt in continuing to use “thrombolytic drugs” as
a first choice, even in recurring episodes (8).
The presence of periprosthetic pannus can contribute to a partial
response to the thrombolytic drug therapy.
In our patient was noticed no allergic reactions.
A streptokinase obtained by means of recombinant-DNA (rSK) has been
evaluated previously in two clinical trials in acute myocardial infarct (AMI)
patients. In the first trial, 224 patients were randomized to receive rSK or
natural streptokinase (nSK). Both groups behaved similarly regarding coronary
patency at eight days after thrombolysis and the changes induced on fibrinogen
degradations products, and thrombin time (9). They were also similar with
respect to anti-SK antibodies titer and their anti-SK neutralizing activity
(10,11).
Streptokinase (SK) is a 47 kDa protein produced by various strains of
hemolytic streptococci and is a potent activator of the fibrinolytic enzyme
system in humans. SK is in widespread clinical use to treat acute infarction
because of its function as an activator of vascular fibrinolysis. Since
streptococcal infections are common, normal individuals are immunized with SK
and antibodies (Abs) to SK can be detected in most of them. This therapy
generates significant T-cell responses to SK and the neutralizing capacity of
the Abs rises significantly. Neutralizing Abs reduces the efficiency of
thrombolytic therapy and may cause allergic reactions (12).
Incidence of rethrombosis is approximately 20% of the patients treated with
thrombolysis (13). Torrado and co-workers recommend treatment of rethorombosis with further administration of
thrombolytics (3). Lengyel have reported a 75% rate of success in recurrent
prosthetic heart valves thrombosis treated with a second thrombolytics administration (14).
Shapira and collegues evaluated the effectiveness and safety of
thrombolytic treatment in stuck bileaflet heart valves in the absence of risk
thrombi. In 12 patients they had 83, 3 % of success with 25 % of rethrombosis.
All recurrent episodes were treated successfully with thrombolytic therapy.
They concluded thorombolytic therapy is highly successful and safe, both in the
primary episode and in recurrence (15).
In our case with a right-sided mechanical prosthetic valve due to
correction of an EA, where the incidence of thrombosis is high, we decided
thrombolytic therapy as first choice of treatment because there were no
contraindications and the previous knowledge of effectiveness and safety of
thrombolysis, also because we share the concept that it constitutes the first line of treatment in prosthetic heart valve thrombosis
independently of functional class and size of thrombus when there are no
contraindications. To trhe best of our knowledge this is the first such a case
report in the literature.
REFERENCES
1.
Mair DD. Ebstein's
anomaly: Natural history and management. J Am Coll Cardiol, 19:1047-1055, 1992.
2.
Celermajer DS, Bull C,
Till JA. Ebstein's anomaly: Presentation and outcome from fetus to adult. J Am
Coll Cardiol, 23:170-175, 1994.
3.
Torrado E, Ferriz JA,
Prieto MA, Rodríguez JJ, Alvarez JM, Vera A, et al. Thrombolysis
of thrombosed heart valve prostheses: presentation of 2 cases and review of the
literature. Rev Esp Cardiol, 43:345-351, 1990.
4.
López
H, Cáceres FM, Morlans K, Fagundo H, González N, Marrero MA, et al. Thrombolytic therapy with recombinant
streptokinase for prosthetic valve thrombosis. J Card Surg, 17:387-393, 2002.
5.
Lengyel M, Fuster V, Keltai M, Roudaut R,
Schulte HD, Seward JB, et al. Guidelines for management of left-side prosthetic
valve thrombosis: a role for thrombolytic therapy. Consensus Conference on
prosthetic valve thrombosis. J Am Coll Cardiol, 30:1521-1526, 1997.
6.
Alpert J. The thrombosed prosthetic valve.
Current recommendations based on evidence from the literature. J Am Coll
Cardiol, 41:659-660, 2003.
7.
Lengyel M. Thrombolysis should be regarded
as first-line therapy for prosthetic valve thrombosis in the absence of
contraindications. J Am Coll Cardiol, 45:325, 2005.
8.
Echarte
JC, Pedroso J, Hidalgo J, Barrera JD. Trombolisis reiteradas en
prótesis tricúspide de Bjork-Shiley. Rev Cubana
Cardiol Cir Cardiovasc, 10:44-49, 1996.
9.
The TERIMA Group Investigators. Multicenter, randomized,
comparative study of recombinant vs. Natural streptokinase in acute myocardial
infarct. Thromb Haemost, 82:1605-1609, 1999.
10.
Mainet D, del Rosario M, Toruncha A. Similar, more than
6-months persisted, antibody and neutralizing activity responses in patients
with acute myocardial infarction treated with recombinant or natural
streptokinase. Fibrinolysis & Proteolysis, 12:301-309, 1998.
11.
The
TERIMA Group Investigators. National Extention of Thrombolytic Treatment with
Recombinant Streptokinase in Acute Myocardial Infarct in
12.
Reyes O, Torrens I, Ojalvo
AG, Seralena A, Garay HE. Profiling the immune
responses of human patients treated with recombinant streptokinase after
myocardial infarct. Mol Divers, 8:251-256, 2004.
13.
Rodaut R, Lafitte S, Rodaut MF, Courtault C, Perron
JM, Jais C, et al. Fibrinolysis of mechanical prosthetic valve thrombosis: a
single center study of 127 cases. J Am Coll Cardiol, 41:653-658, 2003.
14. Lengyel M.
Management of prosthetic valve thrombosis. J Heart Valve Dis, 13:329-334, 2004.
15.
Shapira Y, Herz I, Vaturi M, Porter A, Adler Y,
Birnbaum Y, et al. Thrombolysis is an effective and
safe therapy in stuck bileaflet mitral valves in the absence of high risk
thrombi. J Am Coll Cardiol, 35:1874-1880, 2000.
Published by the Canadian Society for Pharmaceutical Sciences.
Copyright © 1998 by the Canadian Society for Pharmaceutical Sciences.